Surgical Treatments For Lymphedema
The aim of this page is to provide the reader with an overview of the surgical work-up and treatment options for lymphedema. Standard treatment for lymphedema has been complete decongestive therapy (CDT).
This is a combination of physiotherapy and compression garments. It can control symptoms and may slow disease progression. However, new surgical therapies have been developed that may halt or even reverse the progression of lymph edema. These include liposuction, lymphaticovenous anastomosis (LVA), and vascularized lymph node transfer (VLNT). These surgeries can be performed in isolation or in combination.
In order to determine whether someone is surgical candidate, we perform three imaging tests. These include lymphoscintigraphy, florescence imaging, and magnetic resonance imaging.
Imaging Tests 1 – Lymphoscintigraphy
Lymphoscintigraphy is a nuclear imaging study done in the hospital radiology department. The limb is injected with a tracer. The tracer, technetium, is a substance that enters the lymphatic vessels and is carried to the lymph nodes. It can be followed by the radiologist as it passes through the body. A series of images are taken over a period of several hours. This allows for detection of abnormalities of the lymphatic system regardless of the cause. It may demonstrate slow or absent lymph flow and areas of reflux (backflow) though the lymph vessels.
Lymphoscintigraphy can also reveal abnormalities of the lymph nodes themselves. The health of the lymphatic system is scored based on the migration of the tracer through the limb, the presence or absence of backflow, and the number of healthy lymph nodes present. Patients with impaired lymphatic flow or a reduction in the number of functional lymph nodes may benefit from LVA and VLNT surgery.
Imaging Tests 2 – Florescence Imaging
Fluorescence imaging, also known as near infra-red florescence, is done in the hospital or office setting. A tracer is injected at the base of the fingers to assess functioning of the lymphatic vessels. The tracer used is indocyanine green or ICG. Using a specialized near infra-red fluorescence camera, the tracer is followed as it travels up the arm.
The health of the lymphatic system is scored based on the migration of the tracer through the limb and the presence or absence of backflow. Fluoresence provides a much more detailed image of the lymphatics in the extremity than lymphoscintigraphy, however it only images to a depth of 15 mm below the skin. Lymphedema patients who have superficial functioning lymphatic vessels are candidates for LVA surgery, with or without VLNT. Those without may be candidates for VLNT.
Imaging Tests 2 – Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to create detailed images of the entire limb. This will show whether limb swelling is due to lymph fluid, fatty changes or fibrous tissue. Once the swelling is due mainly to fibrous tissue, the changes are irreversible. Using a specialized 3 Tesla MRI, images can also be used to image lymphatics vessels and small veins under the skin. Patients with irreversible fibrous changes may be candidates for liposuction, with or without VLNT.
Prior to the development of newer surgical procedures, surgery was restricted to surgical resection. For this treatment, the diseased skin, fatty tissue, and fibrous tissues is resected and the limb is then covered with skin grafts. This leads to significant disfigurement. Surgical resection is reserved for patients with end stage lymphedema where the limb has become swollen and hard. In these individuals, the lymph fluid has been replaced by thick fibrous tissue, and consequently, they suffer from severe, recurrent infections. Newer surgical treatments are designed to treat lymphedema at much earlier stages of the disease. These treatments include liposuction, lymphaticovenous anastomosis (LVA) surgery, and vascularized lymph node transfers (VLNT).

Liposuction Treatment
Liposuction may have a role for patients with no functioning lymphatics where the limb remains soft. In these individuals, the swelling is due mainly to lymph fluid and fat with some fibrous tissue. Using liposuction, the lymph and fat are removed from the limb in order to directly reduce its size and weight. Patients who undergo liposuction can expect to have a significant reduction in the size of the limb. However, liposuction does not improve the functioning of the lymphatic system. Patients must continue physiotherapy and garment use to avoid recurrence.
Lymphaticovenous Anastomosis (LVA) Surgery
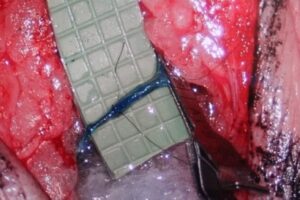
Lymphaticovenous anastomosis surgery (LVA) surgery improves the function of the lymphatic system by connecting lymph vessels to nearby veins. A damaged lymphatic vessel may not be able to carry lymph fluid all the way up the limb to the lymph nodes (Figure 1). As a result, lymph fluid spills out into the tissue of the arm. By creating a connection between a lymphatic vessel and a vein, the lymph fluid can drain into the vein and be carried out of the arm. These connections are created just below the skin though small 2-3 cm incisions. The surgery can be done under general or local anesthetic and patients can return home the same day.
In order to undergo LVA surgery, patients must have some functioning lymph vessels and lymph nodes. The procedure can slow the progression of lymphedema or even reverse the process. Patients with earlier stage lymphedema may have a significant improvement in symptoms with LVA surgery. Studies have shown a partial reduction in arm swelling, decreased rates of skin infections, decreased need for physiotherapy, decreased need for garments, and improved quality of life. The risks of LVA surgery are relatively low as the surgery can be done under local anesthetic.
Vascularized Lymph Node Transfers (VLNT)
Vascularized lymph node transfer (VLNT) involves surgically removing a group of lymph nodes from one area of the body and transplanting these into the affect limb. The nodes are usually taken from the groin with an artery and vein. This tissue is brought to the affected arm where the artery and vein of the VLNT are attached to an artery and vein in the arm. VLNT surgery requires a general anesthetic and may take 3 – 6 hours. Patients are required to stay in hospital for 3 – 5 days. Although it is unlikely, taking nodes from the groin could lead to lymphedema of the leg.
Patients with arm swelling that is still soft and who have some functioning lymphatic vessels may have significant improvement from VLNT. When possible, LVA surgery is done at the same time. Studies have shown VLNT may lead to a reduction in the size of the limb, the number of infections, the need for physiotherapy, and the need for garments. Risks include those of general anesthesia, infection, failure of the lymph node transplant, and the development of lymphedema of the leg.
Lymphedema is a complex and chronic problem. Traditional treatment has relied on physiotherapy and compression garments to control symptoms and delay disease progression. In the past, surgery was used only in dire cases. The development of LVA and VLNT surgeries provides new hope for patients. These procedures work by repairing the damaged lymphatic system and have the potential to reverse the disease process.
About Dr. Anzarut
Dr. Alexander Anzarut is a plastic surgeon in Duncan, British Columbia. He has been training at the European Center of Lymphatic Surgery, University of Brussels. It is a referral center for patients from Europe. Under the leadership of Drs. Hamdi and Zeltzer, the program has developed imaging protocols, surgical techniques, and treatment algorithms to advance the care of individuals with lymphedema. Using quality of life outcome measures they have been able to show improvements in quality of life after lymphedema surgery. In well selected patients, surgery has decreased or eliminated recurrent skin infections, the need for physiotherapy and garment use. In January 2016, Dr. Anzarut will return to Duncan and begin a lymphedema program.
Figure 1. LVA surgery showing a surgical connection between a lymph vessel and vein